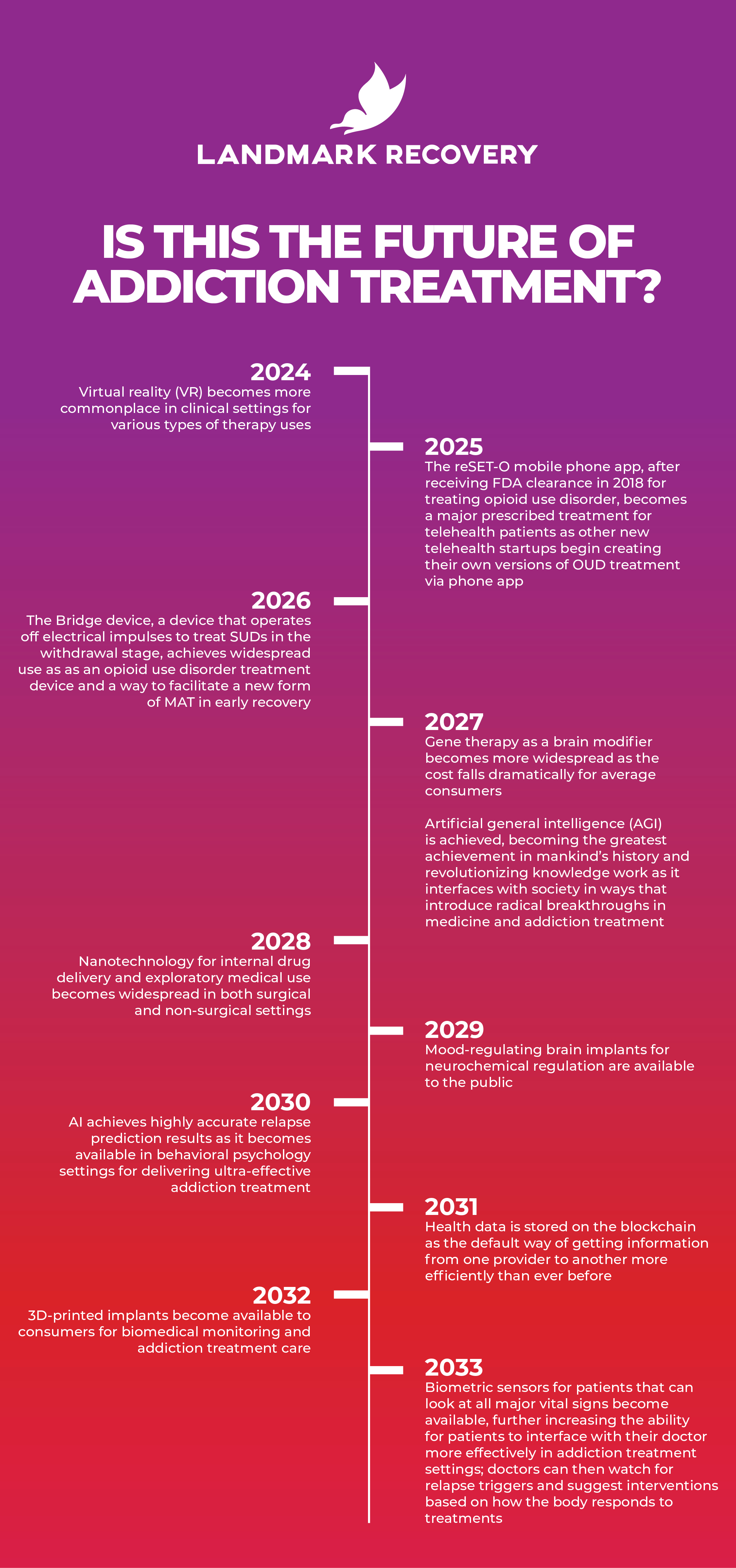
The future of addiction treatment is bright, especially with new technologies on the horizon that could improve, supplement or streamline the way we deal with substance use disorder (SUD). Some of the most exciting developments are coming from the incorporation of artificial intelligence into the medical professional workflow, digital health solutions that bring the expertise of a doctor to your phone, the ability to change our genetic makeup for the better, and alternative therapies that offer other promising ways forward.
Note: All images in this article are generated using artificial intelligence.
Artificial Intelligence (AI) Applications for Addiction Treatment
Doctor’s Assistant
Large language models (LLMs), like GPT, are predictive AI systems that provide high-level output based on sentences or data you feed them. GPT, the base model of OpenAI’s LLM series, works by predicting “tokens” based on questions or sentences you provide. If you ask it to write a letter to a patient’s insurance questioning a denial on behalf of the patient, then it can do so for you.
LLMs like GPT may one day be used to help in clinical and administrative roles, freeing up doctors to be more productive and effective in treating patients suffering from addiction. Incorporating an interactive LLM that’s trained on clinical data makes the job of a psychiatrist, therapist, or psychologist much more effective. A LLM could complete other types of paperwork or offer clinical advice from a vast database that amounts to the sum of human medical knowledge.
In December 2022, ChatGPT, the most popular LLM chatbot program in history, was administered portions of the US Medical Licensing Exam (USMLE). ChatGPT performed at or near the level required to pass the test without specialized training data. This offers one potential hint at the true power of a LLM in a clinical environment as a clinical decision-making assistant. AnsibleHealth, the company responsible for publishing the findings, made the preprint available through medRxiv.
AI Therapist for Addiction
A LLM can be trained on personal input to act as a highly personalized therapist. If you were to upload the entirety or parts of your childhood diary, you could train a LLM to act as a past version of you with which you could discuss and learn to move past childhood trauma or other adverse events. LLMs, like PsychGPT, may one day be able to help therapists address patients’ personal feelings and help diagnose mental illnesses in a clinical environment.
Drug Synthesis for MAT and Understanding Biochemistry
AlphaFold, an AI system developed by DeepMind Technologies that can predict the structure of proteins in the body (or any other organic environment), has been used to help discover new drugs that more effectively target issues like cancer or other diseases. Soon, AI systems like AlphaFold could be utilized in addiction treatment settings to create medication-assisted treatment (MAT) drugs that more effectively target biochemical causes of addiction in certain patients or treat mental illness.
Since a complete understanding of human metabolism is still largely a mystery to scientists, AI systems like AlphaFold can also assist scientists in finding new explanations of human behavior and biochemistry. Since addiction impacts brain chemistry as well as neurotransmitter creation and absorption, this could help scientists find new explanations for why some people suffer from addiction more so than others.
Digital Health Solutions
Sobriety Apps
Many of those interested in the “sober curious” movement are tracking their alcohol consumption habits, or lack of alcohol consumption, with purpose-built apps. Some of the most popular apps available are I Am Sober, Reframe, and Sober Grid. I Am Sober has over 100,000 reviews on the Apple App Store and offers a socially connected experience for users to discuss their journey among each other.
Telehealth Expansion
Since the start of the COVID-19 pandemic, many regulations placed on the operation of telehealth companies and services were rolled back. According to McKinsey & Company, “telehealth use has increased 38 times from the pre-COVID-19 baseline.” The Centers for Medicare and Medicaid Services (CMS) reported that telehealth services helped to reduce opioid overdoses beyond what they would’ve been had it not been available. While many of the deregulatory measures passed by the United States government were temporary, some of them were permanent, meaning that telehealth services are more available now than ever. If these services can help individuals suffering from opioid use disorders avoid overdose, then they may be able to help anyone suffering from an SUD in the future get the help they need.
Remote Health Monitoring
Remote health monitoring opportunities are becoming available for healthcare providers in addiction treatment fields. New startups, like Sonara Health, are popping up across the country as a new way to provide opioid use disorder (OUD) MAT for patients allowed to self-administer drugs like methadone. Due to the high abuse potential for methadone, Sonara is pioneering a new way of ensuring compliance over a phone while allowing those who can self-administer doses to do so from the comfort of their homes. This is how they also keep the cost of traveling to and from a methadone clinic as low as possible to patients. Behavioral Health Business described the process:
“Founded in 2020, Sonara Health uses a mobile web page optimized for the low-quality smartphones provided via federal and state assistance programs and taper-aware labels to track methadone medication compliance. Patients scan a unique QR code on the label before opening the dosage bottle. Then they film themselves taking the medication and read a prompt to prevent the medication diversion practice of ‘cheeking’ and ensure the patient swallowed the medication.”
Personal Health Data on the Blockchain
Storing healthcare data on a blockchain format can ensure that health data are securely stored, yet available to all healthcare professionals that might need to access them without altering it. Without access to special shared code, non-healthcare individuals won’t be able to access personal data. This can ensure greater compliance between providers and more intelligent analysis of relevant data to treat patients more easily, especially those who might have a hard time transferring data between addiction treatment providers.
Genetic Technology
Genetic Profiling
Genetic profiling helps doctors treat patients better by creating a profile for a particular patient to see why and how their body reacts to certain stimuli like abused substances, for example. This, in addition to predictive AI that detects future health events based on human behavior, can help new treatments be developed that are further individualized to each patient.
Targeted Cell Therapy
Some biotech companies have developed ways to use genetic research for creating customized, individualized cell therapies for patients who need something more targeted. For example, some cell therapy research companies use genetic information from malignant tumors to target other instances of tumor growth more effectively in the body. They examine information contained in the tumor sample and manufacture new cells for injection into a patient’s body to fight the cancer or a disease. The National Institutes of Health (NIH) defines cell therapy using an example of how cancer can be fought with genetic modification:
“Gene-modified cell therapy involves removing cells from a patient’s body, in order to introduce a new gene or correct a faulty gene in vitro. The modified cells are then put back into the body. An example of this approach is chimeric antigen receptor (CAR)-T cell therapy. In CAR-T cell therapy, a gene is introduced to the patient’s T cells, which are a kind of immune cell, in vitro using a vector. The additional gene changes the T-cells in a way that enables them to recognize and attack specific cancer cells.”
While currently this tech is expensive and used in very narrow circumstances, this technology may one day be used in individualized, genetically targeted interventions for patients who need a more effective SUD intervention. Cell therapy could take advantage of the way their brain produces chemicals that respond to abused drugs. Perhaps doctors can provide genetically modified genetic information via cell therapy for modifying genetic sequences that predispose someone to developing a SUD.
CRISPR
A more effective way of delivering genetic instructions to change the way the body works is through a process called CRISPR. CRISPR (pronounced “crisper”) is a type of genetic editing process that utilizes a special protein for genetic cutting and splicing; it can be used to edit brain receptors that are activated when a drug is used. The brain’s mu opioid receptor, or the brain receptor that causes respiratory depression (reduced breathing rate) in opioid users can be deleted or edited to stop overdoses. A Journal of Physiology publication from 2020 showed that this was possible in lab mice.

Alternative Treatment
Psychedelic Therapy
The use of previously illegal psychedelic drugs are becoming more commonplace in therapy environments. This class of psychotherapy drugs includes ketamine, LSD, psilocybin, and MDMA. Johns Hopkins University, home of the Center for Psychedelic and Consciousness Research, has become an unwitting pioneer in the field by conducting some of the most comprehensive clinical trials and studies on their use in fighting addiction and conducting psychotherapy.
In 2020, a study by Johns Hopkins University showed that two doses of psilocybin significantly relieved depression in participants. This is a sign that one day magic mushrooms may be used in clinical settings to treat root causes of addiction in effective ways that rival pharmaceutical interventions with prescription drugs like selective serotonin reuptake inhibitors (SSRIs).
Psychedelics Improving Neuroplasticity
Psychedelic substances may improve neuroplasticity to an extreme degree during therapy sessions, allowing the brain to make real, lasting changes to something being addressed during a session. When those suffering from a SUD use substances over a long period of time, the brain adapts to the biochemical changes resulting from the drug use. These adaptations in turn damage the brain’s ability to ignore the reward circuitry’s incentivization, meaning that compulsive behavior increases and cognitive control decreases. The damaged brain cell pathways can negatively affect a patient’s ability to overcome an addiction. Psychedelics have been shown to build up the brain’s ability to “heal” from this kind of damage by stimulating neuroplasticity; increased neuroplasticity means that the brain can form new brain cell connections, make current ones more effective, and recover from maladaptive patterns.
A 2015 proof-of-concept study published in the Journal of Psychopharmacology showed notably positive effects when the use of psilocybin was introduced in a clinical environment geared toward treating alcohol use disorder.
“The intensity of effects in the first psilocybin session (at week 4) strongly predicted change in drinking during weeks 5–8 (r = 0.76 to r = 0.89) and also predicted decreases in craving and increases in abstinence self-efficacy during week 5. There were no significant treatment-related adverse events. These preliminary findings provide a strong rationale for controlled trials with larger samples to investigate efficacy and mechanisms.”

The use of psychedelics outside of a clinical environment is strongly discouraged, as their use is illegal and uncontrolled by a medical professional.
Anti-SUD Vaccines
Researchers that work as part of the NIH’s Helping to End Addiction Long-term (HEAL) initiative are investigating the viability of a vaccine that helps the body create antibodies against opioids. The antibodies created by the immune system after vaccination would bind to the opioid compounds and keep them from crossing the blood-brain barrier. The goal of the vaccine would be to prevent overdose symptoms in those who take opioids. It blocks the opioid high and stops respiratory depression.
Is This the Future of Addiction Treatment?
Learn More
To learn more about how Landmark Recovery helps those in need of effective addiction treatment, give us a call at 888-448-0302 today. We’re on a mission to save a million lives in the next one hundred years in a safe and effective manner. Our evidence-based addiction treatment aims to incorporate new FDA-approved treatments to become even more effective in treating addiction.

Choose Recovery Over Addiction
We're here 24/7 to help you get the care you need to live life on your terms, without drugs or alcohol. Talk to our recovery specialists today and learn about our integrated treatment programs.




