This past month has seen the passing of two prominent figures in the social sphere of popular culture whom, to the casual observer, seemed to have everything. Kate Spade, international business mogul and fashion designer, and Anthony Bourdain, celebrated television chef and world traveler, were both successful, wealthy, beloved celebrities who seemed to have been dealing with darker, more troubling emotions than anyone outside of themselves knew about.
What are Deaths of Despair?
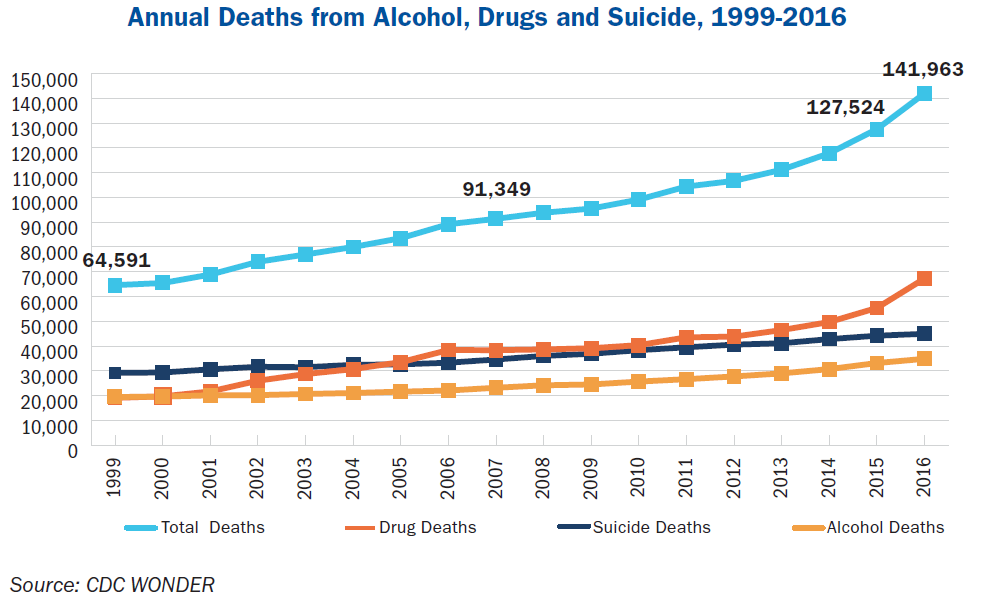
It’s no secret, but it always bears repeating that wealth, success, and external signs of happiness are not insulants from suicidal ideation. Anyone can be struggling with despair, no matter what level of society they are or how happy they appear to be on the outside. Shocking statistics from the CDC have shown that the national suicide rate has been increasing over the last decade, jumping by more than 25% from 1999 to 2016. In the latter year, we lost nearly 45,000 lives to suicide. However, deaths from suicide are not the only rising statistic related to a growing problem of despair in the United States.
In 2016, 142,000 Americans died from alcohol-induced fatalities, drug overdose, or suicide, translating to one person every four minutes. These three causes have contributed to the unprecedented fall in life expectancy between 2015 and 2016, with the expectation that our nation is on track to lose more than two million people by 2025. Between 1999 and 2016, the death rate from alcohol-related causes rose by 55%.
We can find more evidence of an increasing mental health and substance abuse crisis by examining types of hospitalizations over the last ten years. Admissions for mental health and substance abuse were the only categories of hospitalizations that increased from 2005 to 2014, with opioid-related inpatient stays rising 64% from 2009 to 2014. Additionally, drug-use related hospital stays for mothers and newborns included a 135% increase in stays related to opioids.
What’s more, the last decade of our history has been rife with tragic mass shootings that have claimed lives and irrevocably harmed communities. Gun homicide rates in the U.S. are 25 times higher than any other country among other high-income countries. According to research by prominent criminologist Grant Duwe, at least 59% of the 185 public mass shootings that took place in the United States from 1900 through 2017 were carried out by people who had either been diagnosed with a mental disorder or who demonstrated signs of severe mental illness before the attack.
Our nation is facing a mounting crisis related to alcohol and drug misuse as well as a mental and behavioral health crisis that can be glimpsed in the rising suicide rate and definite increase in the frequency and body count of mass shootings. If this public health crisis were related to the spread of disease, our country would call for a nationwide response to combat the epidemic. However, because mental health and addiction are taboo subjects that are either pushed under the rug or relegated to victim blaming, it’s challenging to accrue a coordinated response from the government that can adequately and comprehensively address the situation. Here is a comprehensive outline for combating America’s crisis.
Preventative Measures
To stem the rising tide of despair related deaths in the United States, we need to work with hospitals, healthcare systems, and businesses to implement a coordinated solution. Studies have shown that prevention programs can be cost-effective and save more lives than purely punitive programs. Preventative measures should include better mental health screening and reduced access to lethal means.
Screening for Mental Health
Screening for substance abuse, suicidal ideation, and other mental health indicators is a critical step that healthcare systems and businesses can implement to begin saving lives. The Substance Abuse and Mental Health Services Administration has a specific outline known as the SBIRT method (Screening, Brief Intervention, and Referral to Treatment) that has been linked to lower healthcare costs, lower rates of drug and alcohol misuse, and reduced risk of trauma. School, businesses, and healthcare organizations can use this tool to help identify individuals at risk for suicide or developing a substance abuse disorder. The process is as follows:
SBIRT Method
- Screening: Involves screening patients on a regular basis using age-appropriate questionnaire
- Brief Intervention: Involves an intervention with patients that show at-risk behaviors by introducing feedback on their unhealthy behaviors while educating them about available tools and resources involved with substance abuse and suicidal ideation.
- Referring for Treatment: If a patient is considered at high risk, they are referred for further professional assessment and services.
Reduce Access to Lethal Means
A proven successful method of reducing access to firearms and unused medication is the Counseling on Access to Lethal Means (CALM) approach. One study in Colorado on this intervention method found that parents of children being treated for suicide risk made significant changes in their behavior surrounding safe storage after undergoing the program. In follow up interviews, 76% of parents reported that medications were safely locked up (compared to 10% beforehand) and 100% of those with guns said that their arms were securely locked up (compared to 67% previously).
Another solution to reducing access to medications is implementing medication “take back” programs that prevent drug misuse by encouraging all excess medicines to be deposited in safe disposal locations. At least 53% of people who misuse prescription drugs get them from family and friends, so by encouraging drop box disposal methods states can reduce the harm associated with an overabundance of prescription drugs lying around.
Legalizing Marijuana
The evidence thus far has shown that marijuana legalization is not only working but is benefiting local populations with unexpected additional effects. By comprehensively regulating marijuana for adult use, states are saving money on criminal arrests, earning tax revenue, distributing more wealth to school funding, reducing opioid overdose rates, and protecting the public. Also, the industry is currently employing more than 200,000 full time and part time employees in the states.
- In states with medical marijuana access, overdose death rates are, on average, 25% lower than states with no legal access to marijuana.
- Legal access to medical marijuana has been associated with 23% reduction in opioid dependence and 15% fewer treatment admissions.
- Marijuana sales in Washington generated $315 million in tax revenues in the 2016-2017 fiscal year. 25% of tax revenue is given to substance use disorder treatment, education, and prevention.
- Marijuana sales generated almost $600 million for Colorado since sales began in 2014. Between 2015 and 2017, Colorado distributed more than $230 million to the Department of Education.
- Oregon collected more than $70 million by 2016-2017 fiscal year, more than twice the predicted revenue. 40% of all tax revenue goes towards public education, and 20% to alcohol and drug treatment.
- In no state have vehicular crash rates or marijuana-related hospitalizations increased outside of national averages.
Community Efforts
Our local communities, families, and work organizations are on the front lines when it comes to combating depression, anxiety, suicidal ideation, and substance abuse disorders. We need to work to ensure that our communities value strong social ties and healthy friendships, as well as work with organizations to promote programs that help stem the tide of drug and alcohol addiction and help families heal.
Social isolation, alienation, and shame are all fertile breeding grounds for suicidal ideation and drug and alcohol addiction. Sociologist Emile Durkheim once stated the connection between suicide and alienation: “Melancholy suicide. —This is connected with a general state of extreme depression and exaggerated sadness, causing the patient no longer to realize sanely the bonds which connect him with people and things about him. Pleasures no longer attract.”
Healthcare systems can work with communities to help reduce harm, provide support, and educate people on topics of addiction and mental health. For example, some hospitals provide training for first responders and police officers on how to safely administer the anti-overdose drug Naloxone.
The Massachusetts General Hospital Center for Community Health and Improvement launched four coalitions focused on preventing substance abuse disorders, including take-back programs, naloxone distribution, increasing connections to treatment through recovery coaches, and screening patients for substance abuse. The Charlestown Drug Court Coalition has seen some notable success, with Emergency Medical Service responses for heroin overdoses decreasing 62% from 2003 to 2010 and drug-related deaths decreasing 78% between 2003 and 2008.
Increasing Access to MAT
Although MAT, Medication Assisted Treatment is one of the National Principles of Care for Substance Abuse and endorsed by all major government health agencies and experts in the field, it is still widely stigmatized and underused in the medical profession. A Blue Cross Blue Shield study found that while the rate of patients diagnosed with an opioid use disorder between 2010 and 2016 increased, the rate of those receiving MAT did not grow at a comparable rate.
MAT deserves credibility as a viable and effective solution to curbing addiction. One 2015 study found that treatment of opioid abuse with MAT was associated with lower monthly healthcare expenditures, with patients 50% less likely to relapse compared to patients using non-MAT recovery.
Increasing Access to Behavioral Health Providers
Currently, there are not enough providers of behavioral health care available to most of the country. According to the Substance Abuse and Mental Health Services Administration, 55% of U.S. counties do not have any practicing mental behavioral health workers and 77% report that they have unmet behavioral health needs. Healthcare systems can address these shortages by offering recruitment incentives to behavioral health providers, providing care in teams that include both behavioral health workers and physicians, and implementing innovative approaches such as telehealth to ease geographic and logistic difficulties.
Improving Pain Management and Treatment
While patients should not have to suffer during recovery, it’s essential that doctors administer painkillers in a responsible manner that ensures patients are not substantially exposed to the risk of substance addiction. By following strict guidelines for opioid prescribing, recognizing early signs of opioid dependence, and expanding PDMP’s, physicians can significantly reduce opioid abuse.
Follow CDC Guidelines for Prescribing Opioids:
The guidelines officially supported by the CDC outline the following for treatment that does not include active cancer, palliative, or end-of-life care. Physicians should:
1. Not use opioids as a first-line treatment;
2. Establish goals for pain reduction and function and continue opioid use only if the benefits of opioids towards meeting these goals outweigh the risk;
3. Inform patients of the benefits and risks of opioid use;
4. Begin opioid treatment with immediate-release versions;
5. Use the lowest effective dose when prescribing opioids;
6. Prescribe opioids in short duration for acute pain;
7. Frequently reevaluate the harms and benefits of continued use of opioids;
8. Use risk reduction strategies, such as naloxone;
9. Review PDMP data;
10. Drug test patients before starting opioid therapy and at least annually;
11. Avoid prescribing opioid and benzodiazepine concurrently; and
12. Offer treatment, including MAT, for patients with opioid use disorder.
Harm Reduction Through PDMP’s (Prescription Drug Monitoring Program)
PDMP or the Prescription Drug Monitoring Program is a tool that states can use to address prescription drug diversion and abuse. Each program differs from state to state, but the general idea is that you have a database tracking prescriptions to potentially identify patients who may be doctor shopping, doctors who may be over-prescribing medications, and patients who could be being co-prescribed medications. If a state requires all its operating physicians to consult the PDMP before prescribing medication, it could potentially reduce the risk of abuse and dangerous co-prescriptions.
Studies on states that implement PDMP’s show that they have reduced opioid prescription rates by 8% and opioid overdose deaths by 12%. Data from the CDC looked at prescription rates nationally and reported that opioid prescriptions rose 10% from 2006 to 2010, and decreased by more than 13% from 2012 to 2015. Examinations of prescription lengths showed that patients were at risk for abuse after using them daily for more than five days, and were more unlikely to discontinue after using for more than 90 days.
There are 29 states currently using PDPM strategies to reduce the risk associated with prescription drug abuse. Over the past decade, more states have succeeded in implementing Prescription Drug Monitoring Programs, which may have played a part in the reduction of opioids prescribed since 2010 which is down to 640 MME’s (morphine milligram equivalents per capita) from 782. While this shows that the tide has been halted, it’s still a far cry from reducing the nearly triple sized number of opioid prescriptions we have now compared to 1999. Another sobering statistic to remind us of the severity of this problem is that the United States opioid prescription rate is nearly four times higher than the amount distributed in Europe.
Currently, opioid prescriptions vary widely across the country, with the highest prescribing locations doling out opioids at nearly six times the rate of other areas. The highest associated risk factors associated with higher prescriptions rates are a more significant percentage of non-Hispanic whites, a higher prevalence of diabetes and arthritis, higher unemployment, and higher Medicaid enrollment.
Conclusion
To adequately address the nation’s rising crisis of deaths relating to suicide, alcohol, and drug use will require a comprehensive treatment approach that involves health care systems, communities, and businesses to rally and face the problem head-on.
At Landmark Recovery, we incorporate leading techniques and methods for giving the highest quality treatment available to our patients. Our program is built on a foundation of love and support. Our drug and alcohol recovery centers are fully equipped and staffed to help you or a loved one overcome a substance dependency.

Choose Recovery Over Addiction
We're here 24/7 to help you get the care you need to live life on your terms, without drugs or alcohol. Talk to our recovery specialists today and learn about our integrated treatment programs.