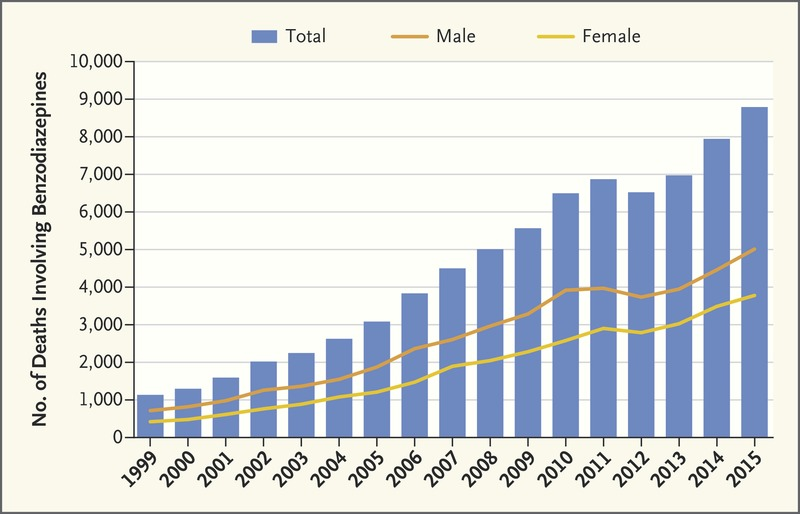
Between 1996 and 2013, the number of adults who filled a benzodiazepine prescription increased by 67% from 8.1 million to 13.5 million, while the number of benzodiazepines more than tripled from 1.1 kg per 100,000 adults to 3.6 kg. The National Institute on Drug Abuse attributed more than 8791 deaths from benzo overdose in 2015 compared to 1135 in 1999, translating to growth roughly 40 times that of the US population in that period.
Facts To Know About Benzodiazepines
Despite these numbers, more attention has been given to the opioid epidemic, but with valid reasoning. Over 3/4ths of deaths from benzos involved mixing with an opioid. However, benzodiazepines growth in the American marketplace and the subsequent number of deaths have been just as startling as opioids. Between 1991 and 2009, Medicaid expenditures on benzodiazepines increased by nearly $40 million, and rates of co-prescribing opioids and benzos nearly doubled from 2001 to 2013.
In 2016, the FDA issued a black-box warning (the strictest warning label put out by the Food and Drug Administration to address the potential risks and hazards of taking a substance) regarding the dangers of co-prescribing benzos and opioids.
What are Benzodiazepines
Benzodiazepines, or benzos, are part of the drug family falling under sedatives. All benzos are considered Schedule II-IV drugs by the DEA. Benzos produce similar calming and sedative effects to opioids, but hold significantly less risk for overdose solely by themselves. However, when combined with opioids, both become significantly more lethal. Instead of targeting the opioid receptors, Benzos target the GABA receptor molecules, which are largely concerned with cognitive processes outside of life functions. So instead of potentially shutting down your lungs (like with opioids), you run the risk of mental drowsiness, amnesia, and problems with learning and motor control.
Benzos create feelings of calmness and relaxation. At higher and higher doses, they can induce vertigo, drowsiness, and muscle in coordination. Depending on level and tolerance, benzo effects can last from an hour or two to more than a day. Other sedatives and opioids will suppress the nervous system and potentially stop your breathing, but benzos do not carry this risk. While these drugs are intended to help alleviate symptoms of anxiety, nervousness, restlessness, and insomnia, when improperly used, they can create these exact symptoms.
Common Benzodiazepines
- Xanax (Alprazolam)
- Klonopin (Clonazepam)
- Rohypnol (Flunitrazepam)
- Valium (Diazepam)
- Librium (Chlordiazepoxide)
- Ativan (Lorazepam)
- Dalmane
- Serax
- Tranxene
- Verstran
- Halcion
- Paxipam
- Restoril
History of Benzodiazepines
Benzodiazepines were developed in the 1950’s in New Jersey, specifically in 1957 by chemists working for Hoffman La Roche, a Swiss pharmaceutical and healthcare multinational. The first benzo to be developed was chlordiazepoxide, known as Librium, and was discovered by accident after co-workers noticed there was a “beautiful crystalline” structure leftover during tests for new tranquilizers. After testing the compound, they found it was surprisingly effective at producing sedative and muscle relaxant effects. Librium was released for pharmacological sale in 1960 and was eventually followed by diazepam, known as Valium in 1963.
Prior to Benzos, the most commonly prescribed medication for producing sedation were barbiturates. Barbiturates were developed by German pharmaceutical companies in the early 20th century and became a popular over-the-counter medication during the Great Depression in the United States. Barbiturates were touted as safer than opiates, but these assurances were little more than sales pitches. By the time the U.S. entered World War II in 1941, Americans were consuming more than 1 billion barbiturates per year. Congress finally clamped down in 1951 and required doctors to prescribe the medication, drastically cutting down the number of consumers, and paving the way for chemists to develop the next generation of sedatives that would appear in the form of benzos.
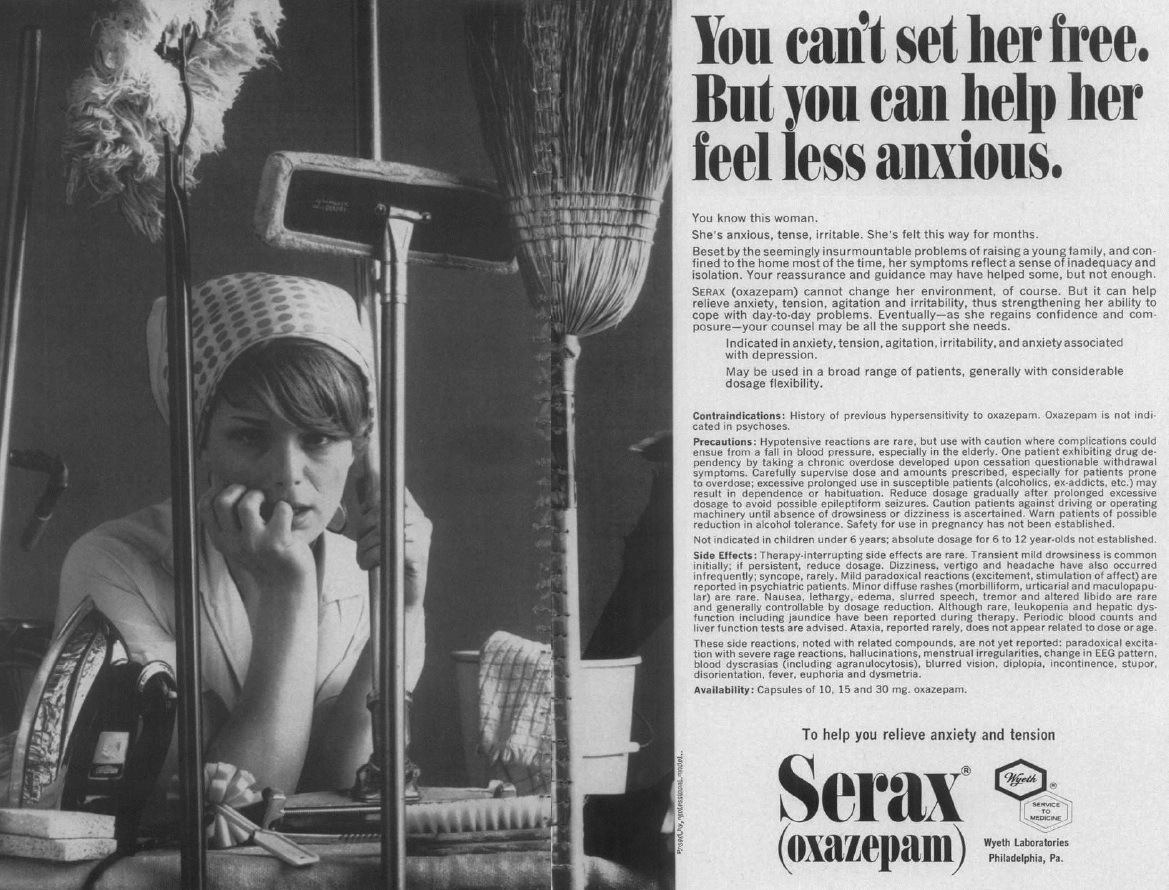
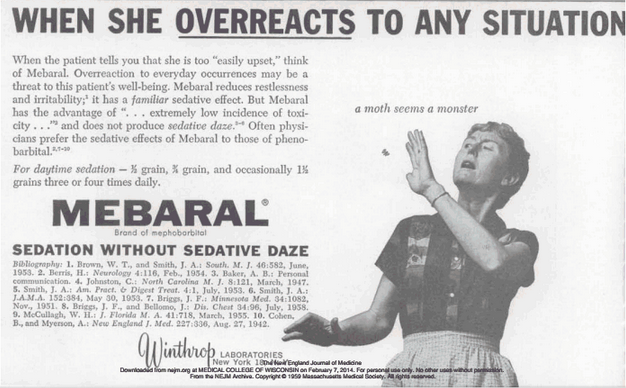
By 1983, there were 17 benzodiazepines available on the worldwide market valued at over $3 billion. By the 1970’s, benzodiazepines were the most prescribed drug in the entire world. It was estimated that one in five of all women and one in ten men in Europe had been prescribed the medication at one point. However, doctors and patients were starting to become more vocal about the potential that benzos had for abuse. Women were prescribed the medication more commonly than men for a variety of issues ranging from insomnia to irritability, and advertising unsurprisingly played off of gender stereotypes to take advantage of this.
Due to lawsuits and growing public awareness surrounding benzodiazepines, prescription levels started to dwindle from 32 million annually to about 18 million (In the UK only). But in America, prescription rates have only risen, especially with the introduction of similar benzos known as the Z-Drugs. The Z-Drugs include zolpidem (Ambien), zaleplon (Sonata, and eszopiclone (Lunesta) in the 2000’s. In the United States, the percentage of adults filling a benzodiazepine prescription increased from 4.1% to 5.6% over the period of 1996 and 2013, with the overdose rate rising from 0.58% to 3.07% in the same period, plateauing after 2010.
Benzos Targeted at Women
As stated earlier, Benzodiazepines were commonly prescribed throughout the middle 20th century to address what advertisers at the time would have dubbed “womanly problems”. The sexist nature of these ads is not surprising given the time period, but it seems as though clinicians are still more inclined to prescribe the drug to women. In 2013, over 61 million benzodiazepines prescriptions were written for women compared with 29 million for men.


According to the Anxiety and Depression Association of America, women are more likely than men to be diagnosed with an anxiety disorder. This could be attributable to many different factors, for example, differences in brain chemistry, ingrained and pervasive societal stereotypes, the fact that women are more likely than men to experience physical and mental abuse, or that women are more likely to seek medical help for mental health than men do.
Benzodiazepine Withdrawal
As with other drugs, Benzodiazepine abuse often results in a physical dependence where the person’s body has trouble functioning without it. Benzo withdrawal is associated with seizures and risk of death along with a number of negative ones that could lead to relapse if you’re not careful. As with alcohol and barbiturates, benzos work by affecting the GABA receptors, and so increase the risk of seizure considerably when withdrawing. Symptoms include:
- Anxiety
- Irritability
- Panic
- Insomnia.
- Sweating.
- Headaches.
- Muscle pain and stiffness.
- Poor concentration.
- Sensory distortions.
- Nausea.
- Heart palpitations.
- High blood pressure.
- Agitation.
- Tremors.
Depending on the severity of the addiction, benzo withdrawal can last anywhere from a matter of days to a whole week, and with acute withdrawal symptoms such as depression, fogginess, and insomnia that can last for months. In severe cases, serious symptoms may occur including seizures and psychosis, though they are far less common. Withdrawing from benzos can also In the initial stages of withdrawal, the brain’s storage of endorphins and dopamine are drastically depleted. The time it takes for these chemicals to naturally replenish and get back into a natural rhythm are what makes the withdrawal so long.
What is Withdrawal Like
In a poll conducted by the narcotic discussion forum Bluelight, Benzodiazepines were voted unanimously as far and away the worst drug to experience withdrawals from. The following testimonials were gathered from the forum and the views expressed are in no way affiliated with Landmark Recovery.
“When using so long, the withdrawals never go away. (for at least 1.5 years from what I’ve read) The withdrawals from just tapering are tough enough and when finally off of them I had anxiety so bad that I’d have reality breaks where I couldn’t tell if I were alive or dead, sort of like dissociation…but in a bad way. About 4 years ago I was able to stay off Clonazepam (from an initial 6 mg prescribed daily dose + recreational doses obtained from doctor shopping or other dealers who’d trade) for 2 months and I never felt so awful in my life…this was after 6 months of tapering also. My hands never EVER were steady, I’d twitch all the time, have mild spasms every couple hours, body would just ‘jump’ every now and again, sharp pains like electricity shooting through the body, out of nowhere I’d get flashes of cold sweat, impossible to get more than four hours of sleep without Ambien, incredible muscle tension and pain (the toughest of the symptoms) and I was ALWAYS stressed out.”
“I’ve gone through serious Opiate withdrawal several times and it never came close to comparing to when I went through Benzo withdrawal from Xanax. It was by far the worst drug-related experience of my life.”
“I’ve been addicted to benzos for about 8 yrs now. I’ve never been able to kick the addiction. The withdrawal is like being tortured non-stop. I was able to taper down to almost being off but the withdrawal was so horrible I said fuck it and went back. Right now I’m down to taking 2 mg every 6 hrs (8mg/day Ativan). It sucks. And you’re always doing the math in your head as to when to pop the next pill so you don’t wait too long and get sick (or a seizure).”
“Benzos for sure, I’m not the first one to mention them here either so a lot of people know the problem, first of all, the withdraw itself if benzo abuse was regular enough, can very easily kill you. But the more common side effects I and probably most others experience, extreme headache, nausea, insomnia, profuse sweating, lots of muscle twitching, spasming, and cramping, among a lot more. Truly hell on earth.”
“Benzo’s are toxic in long-term IMO. Once you are tolerant, they simply become normal. Its like you are not on a drug. They have such deep effects on emotion on learning and you only realize that once you’re off them. I was on them for about 4 years solid but played with them prior. Its four years that are a black hole. I hate that I won’t get it back. So I vow to try and be conscious as much as I can. It’s hard, I’ve had relapses but frankly, benzos terrify me. Utterly.”
“Life is always better without those life destroying little helpers. Challenging, overwhelming, confronting but easier than waking up one day wondering how you slept thru half a decade. Life, damn you, does not sleep. But I’ve learned that fear and uncertainty are manageable. Benzo w/d really isn’t. For me, anything is better than that.”
Harm Reduction Through PDMP (Prescription Drug Monitoring Program)
PDMP, or the Prescription Drug Monitoring Program, is a tool that states can use to address prescription drug diversion and abuse. Each program differs from state to state, but the general idea is that you have a database tracking prescriptions to potentially identify patients who may be doctor shopping, doctors who may be overprescribing medications, and patients who could be being co-prescribed medications. If a state requires all its operating physicians to consult the PDMP before prescribing medication, it could potentially reduce risk of abuse and dangerous co-prescriptions.
Studies on states that implement PDMP’s show that they have reduced opioid prescription rates by 8 percent and opioid overdose deaths by 12 percent. Data from the CDC looked at prescription rates nationally and reported that opioid prescriptions rose 10 percent from 2006 to 2010, and decreased by more than 13 percent from 2012 to 2015. Examinations of prescription lengths showed that patients were at risk for abuse after using them daily for more than 5 days, and were more unlikely to discontinue after using for more than 90 days.
There are 29 states currently using PDPM strategies to reduce the risk associated with prescription drug abuse. Over the past decade, more states have succeeded in implementing Prescription Drug Monitoring Programs, which may have played a part in the reduction of opioids prescribed since 2010 which is down to 640 MME’s (morphine milligram equivalents per capita) from 782. While this shows that the tide has been halted, it’s still a far cry from reducing the nearly triple sized number of opioid prescriptions we have now compared to 1999. Another sobering statistic to remind us of the severity of this problem is that the United States opioid prescription rate is nearly 4 times higher than the amount distributed in Europe.
Currently, opioid prescriptions vary widely across the country, with the highest prescribing locations doling out opioids at nearly 6 times the rate of other locations. The highest associated risk factors associated with higher prescriptions rates are: a larger percentage of non-hispanic whites, a higher prevalence of diabetes and arthritis, higher unemployment, and higher Medicaid enrollment.
In Conclusion
Drug and alcohol addictions are some of the most destructive forces in the world today. Benzodiazepines are extremely dangerous and feed into those powerful addictions. The process of healing ourselves, our families, our communities, and the world at large, starts with recognizing the danger that these substances represent. At Landmark Recovery, we believe in creating a supportive network of love with access to resources that can help you break free from the chains of addiction. Visit our website to learn more about our inpatient rehab centers.

Choose Recovery Over Addiction
We're here 24/7 to help you get the care you need to live life on your terms, without drugs or alcohol. Talk to our recovery specialists today and learn about our integrated treatment programs.