Ketamine is a powerful medication that can induce anesthetic or loss of consciousness.
As a Class III scheduled drug, ketamine is sanctioned for use in hospitals and other medical settings to serve as an anesthetic.
More disturbingly, ketamine is also routinely abused as a recreational drug.
John Abenstein MD, president of the American Society of Anesthesiologists describes the drug as “a miracle in the right hands” while “outside of the clinic, ketamine can cause tragedies.”
Sadly, that sums up many drugs that end up on the black market and used for the wrong reasons. We’ll look today at how ketamine works and how it’s used, both legally and illicitly. We’ll also be briefly examining the controversial idea of ketamine being used to treat depression and addiction.
Firstly, though, some basic facts on the drug.
What Is Ketamine?
Categorized as a dissociative anesthetic, ketamine is an NDMA receptor antagonist.
Other drugs in this category include PCP (phencyclidine), nitrous oxide, and DXM (dextromethorphan). Ketamine is similar in chemical structure to PCP and these dissociative drugs are potent hallucinogens that can induce feelings of detachment from reality.
Ketamine was developed as a replacement for PCP by Parke Davis Laboratories in 1963 and rolled out for veterinary use in Belgium. Ketamine also came out to play on the battlefields during the Vietnam War.
Gaining FDA approval in 1970, ketamine has since been used for anesthetic purposes. In low doses, ketamine can relieve pain, and it’s sometimes used after minor surgery. We’ll touch upon how ketamine is used for medical purposes before pushing on with the core of today’s study, namely ketamine as a drug of abuse.
Legitimate Therapeutic Uses
Ketamine is primarily used by vets and medical practitioners as an animal anesthetic.
Since ketamine suppresses breathing less than most anesthetics and it doesn’t lower blood pressure, it’s also used in hospitals. Ketamine can be deployed as the sole anesthetic for minor procedures or as an induction agent. Due to the hallucinogenic effects, though, it’s seldom used as a primary medication.
In cases of severe injury and traumatic shock, the dissociative sedative properties of ketamine mean it can work well as an emergency solution.
When used for medical purposes, ketamine is either administered through an IV line or injected directly into the muscle.
Medical use cases include:
- Cardiac catheterization
- Controlling seizures
- Diagnostic procedures (eye, ear, nose, throat)
- Emergency surgery in war zone field medicine
- Minor surgical interventions
- Orthopedic procedures
- Sedative in ER
- Skin grafts
Administered by medical professionals in proper doses, ketamine is generally considered safe. Protective airway reflexes are preserved when it’s used as an anesthetic and ketamine stimulates the circulatory system rather than depressing it.
While ketamine undeniably has limited but effective medical applications, it’s perhaps most commonly known as a drug of abuse.
Why, though, would anyone want to voluntarily take a substance capable of knocking out a horse?
Ketamine as a Drug of Abuse
Since the beginning of time, any substance capable of altering the senses has been abused and this is unlikely to change any time soon. Since ketamine can induce wild sensory changes, it’s frequently taking in a club setting.
The drug was used rampantly in the late 1980’s through to the 1990’s in the New York club scene. This excess was immortalized in the 2003 movie Party Monster. Macaulay Culkin stars as Michael Alig, a young promoter and heavy ketamine user whose life spiraled out of control culminating with the murder of his drug dealer.
Use also extends throughout the rest of the world with the drug legally marketed in some countries and prohibited in others.
Ketamine was listed as a controlled substance in the US back in 1999.
How Is Ketamine Used
When used outside medical applications, ketamine is swallowed or snorted. Less commonly, the drug is injected. Smoking this drug with cannabis and/or tobacco is sometimes attempted but rarely repeated.
As always, intravenous injection provides the most direct delivery route with effects kicking in after just 30 seconds. Full effects of ketamine will be felt after roughly 5 minutes when it’s snorted while swallowing the drug delays kick-in by around 20 minutes.
Once the body assimilates to the drug, its effects can last anywhere from 45 minutes to 90 minutes depending on purity levels and the individual. Somewhere around an hour is generally the sweet spot.
What can ketamine users expect to experience? Here things differ substantially from person to person. The size and weight of the user play a part in how strongly the drug takes hold. Purity, quantity and the involvement of any other drugs will also determine the strength and extent of any effects.
Effects of Ketamine
Users can expect to experience any of the following effects after ingesting ketamine:
- Agitation
- Anxiety and panic
- Blurred vision
- Confusion
- Clumsiness
- Decreased sensitivity to pain
- Depression
- Drowsiness
- Feeling detached from the body (this is known as falling into a K-hole)
- Feeling happy and relaxed
- Hallucinations
- Increased blood pressure and heart rate
- Involuntary muscle movements
- Loss of appetite
- Nausea
- Slurred speech
- Violence
- Vomiting
While that might look like a lengthy and unsavory list of effects, the euphoria, floating sensation and hallucinations not dissimilar to those induced by LSD account for its popularity in a dance club setting.
When taken in higher doses, users report falling into a K-hole where they are literally unable to move or communicate, feeling completely distanced from their own body. A casual user unwittingly stumbling down that K-hole is likely to find the experience terrifying. Veteran abusers of ketamine willfully seek out this experience, though.
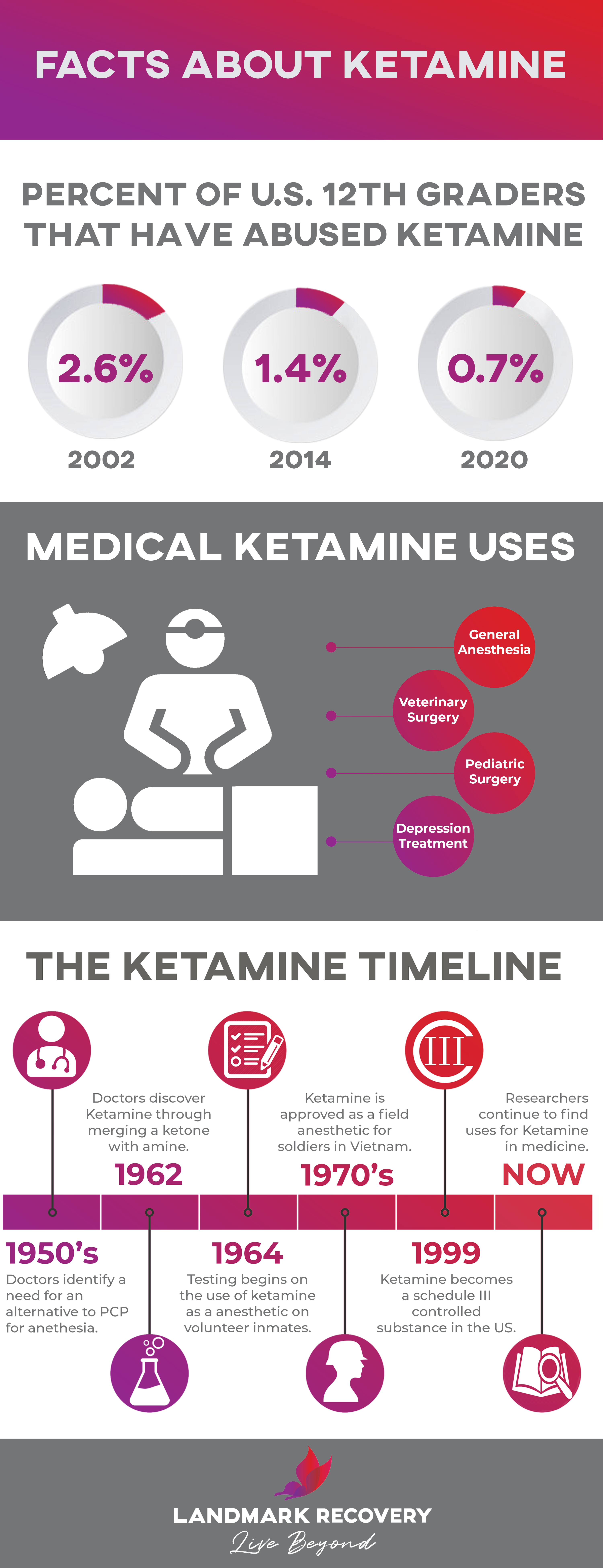
More shockingly than grown adults voluntarily using the drug is the fact that back in 2014, 1.4% of US 12th graders had used ketamine. In 2002, not long after the drug was declared a controlled substance, this figure was even more sobering with 2.6% of those 12th graders questions reporting that they’d used ketamine.
While ketamine is considered so important by the World Health Organization that it’s on their List of Essential Medicines on, it has a range of adverse side effects when used that render it decidedly unsafe when taken outside of a supervised medical setting.
Adverse Effects of Ketamine
Firstly, ketamine is the only addictive psychedelic. Users who acquire a taste for K soon develop the need for much more due to its high tolerance profile. This alone gives it a heightened potential for abuse leading to addiction.
The extreme disassociation caused when users enter the K-hole obviously carries substantial risks depending on where this occurs. This is likened to a bad trip on LSD and is beyond disorienting. Indoors, this can be merely horrifying while if the user is out and about, ramifications are more dramatic. From enhanced vulnerability to assault to an increased risk of accidental injury, it goes unsaid a near-death out-of-body experience on the streets is something to be avoided at all costs.
Other unwanted effects brought about by ketamine include:
- Addiction
- Amnesia
- Flashbacks
- Headaches
- High blood pressure
- Impaired motor function
- Poor concentration
- Psychosis
- Respiratory problems
- Seizures
Coordination, judgment and physical senses can be disrupted for up to 24 hours after use.
When systematically abused, ketamine also has some severe long-term side effects. Bladder and kidney problems can develop. In the worst scenario, this can manifest as ketamine-induced ulcerative cystitis. Stomach pain and sustained memory loss are common.
If addiction sets in, depression can swiftly follow.
Beyond this, it has the capacity to trigger severe mental disorders when used to excess over a prolonged period.
So far, so bad. How about the risks of overdose, though? Can ketamine be lethal?
Ketamine Overdose
The World Health Organization states that ketamine toxicity by itself is unlikely to be fatal.
Ketamine overdose usually occurs when the drug is abused along with other substances, notably alcohol. Of the 1550 ER visits attributed to ketamine over the course of 2011, almost three-quarters of these also involved alcohol.
When used with amphetamines, ecstasy or cocaine, ketamine places a massive strain on the body with the heart motoring at a remarkable and dangerous rate.
That said, the risk of overdose is high. There’s a thin line between a normal dose and one capable of causing an overdose.
If you’re around anyone who has used ketamine and exhibits any of the following symptoms, call 911 immediately.
- Coma or near-death experience
- Fast heart rate
- Inability to move
- High body temperature
Don’t concern yourself with the legal implications of controlled drug use at this stage. All that counts if you suspect a ketamine overdose is summoning medical assistance as soon as possible. Every second counts.
Given this shower of adverse effects, it’s understandable ketamine users soon demonstrate a desire to discontinue use.
Ketamine Withdrawal
For long-term ketamine users, quitting is extremely challenging. The body has developed a marked physical dependence and there’s a significant psychological attachment to the drug, too. This is compounded if the user’s life revolves around club culture and the thought of a night out without chemical assistance seems alien.
Withdrawal symptoms tend to last anywhere from 4 to 7 days and include any or all of the following:
- Anxiety
- Craving for ketamine
- Depression
- Extreme fatigue
- Irregular heartbeat
- Loss of appetite
- Nightmares
- Restlessness
- Sweating and chills
- Tremors
As with any drug or medication, recovery is absolutely possible but will require a great deal of resolve and ongoing effort.
Before closing, we’ll briefly glimpse at the contentious issue of ketamine as a treatment for depression.
The Other Side of Ketamine: Could It Be Used To Treat Depression?
There are several studies indicating that ketamine could have properties capable of treating mood and anxiety disorders previously unresponsive and resistant to treatment. Small sample sizes of studies combined with a complete lack of long-term data as well as questionable data regarding safety has not prevented some doctors prescribing ketamine “off-label.”
The APA (American Psychological Association) advises extreme caution and the FDA have not approved ketamine for the purposes of treating depression.
Researchers, too, have implored doctors to “minimize the risk to patients” before prescribing ketamine on off-label repeat prescription.
It’s clear that evidence is currently lacking but there’s certainly room for further debate and clinical studies. The NIH (National Institutes of Health) is supporting further research into its efficacy counter treatment-resistant depression.
In the UK, ketamine infusions have been used with marked and rapid positive effects to treat depressed patients “for whom nothing else has worked” according to the Department of Psychiatry at the University of Oxford.
This is not the first time it has been tested to explore further use cases. Back in the 1990s, ketamine was tested with statistically significant success on hardcore alcoholics in the USSR by Evgeny Krupitsky. Where only 24% of the control group managed to abstain from drinking for a full year, a staggering 66% of those administered it remained abstinent for that period.
Krupitsky expanded his research when he went to Yale in 1996. A small study tested ketamine on a group of 70 heroin addicts post-detox. Results were again astonishing. Only 2% of the group given a trace amount of ketamine as part of treatment were still clean a year later. 17% of those given a larger dose remained abstinent.
So, ketamine – when properly administered – has a range of benefits and could be considered the psychedelic most likely to be further researched for medical mainstream use. For now, though, don’t expect to be picking up a prescription for K if you’re suffering from mild depression any time soon.
And how about the way in which it’s principally encountered, illegally in a recreational backdrop. What can you do if you or anyone you know is using this drug and you want to kick it aside?
What To Do Next
If you’re unable to stop using ketamine alone, you’ve got many options from residential treatment to intensive outpatient programs.
Call our Indiana treatment center for advice and guidance on all aspects of ketamine, a powerful drug used medically but a potentially lethal substance when abused.

Choose Recovery Over Addiction
We're here 24/7 to help you get the care you need to live life on your terms, without drugs or alcohol. Talk to our recovery specialists today and learn about our integrated treatment programs.