What is considered a dual diagnosis?
Dual diagnosis is a term used when an individual is affected by both substance abuse and mental health simultaneously. It represents an intricate health condition that requires an integrated treatment approach to address both issues effectively. Substance abuse can range from alcohol and drugs like marijuana, opioids, or hallucinogens, to prescription medications.
Mental health conditions, on the other hand, span a wide range, including:
- Depression
- Anxiety disorders
- Schizophrenia
- Bipolar disorder
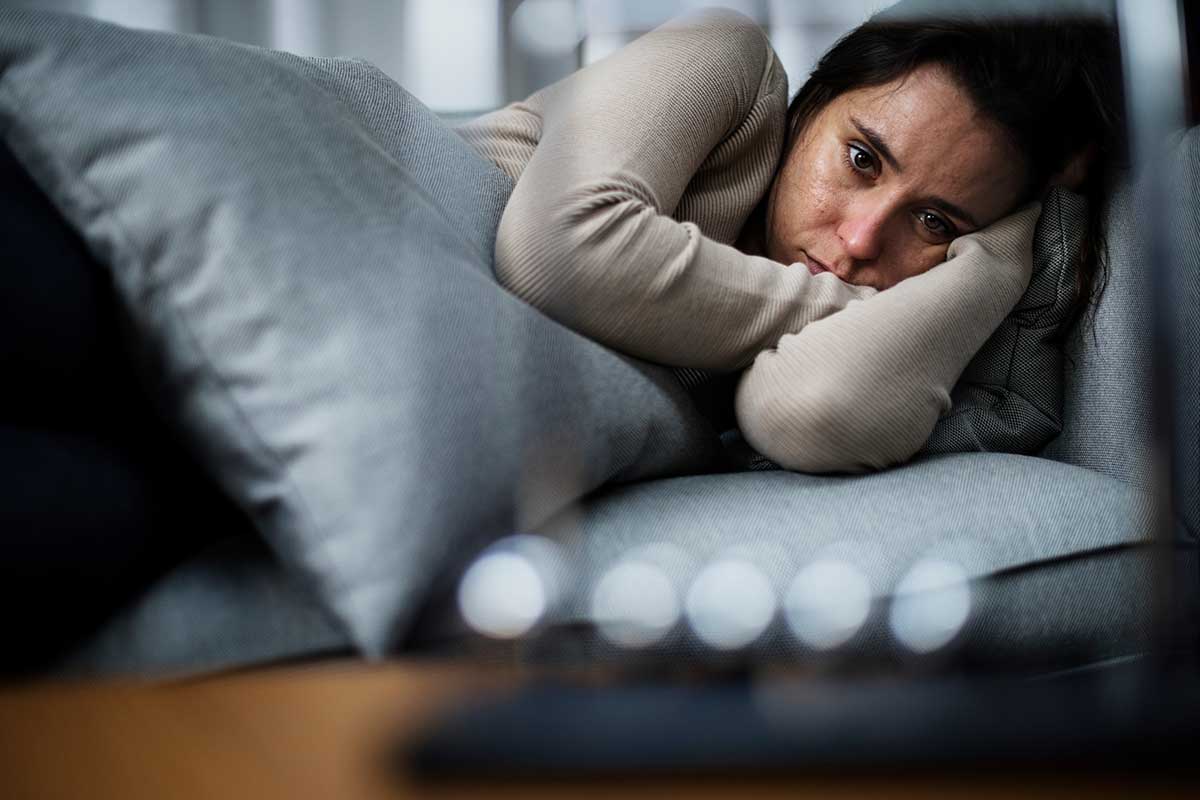
The symptoms of dual diagnosis symptoms can vary widely depending on the specific substance and mental health disorder involved. For instance, a person with alcoholism and depression may experience:
- Extreme sadness
- Loss of interest in activities
- Excessive drinking
On the other hand, an individual with drug addiction and an anxiety disorder may exhibit:
- Excessive worry
- Restlessness
- Drug-seeking behavior
As such, dual diagnosis is a complex condition that demands comprehensive assessment and targeted treatment.
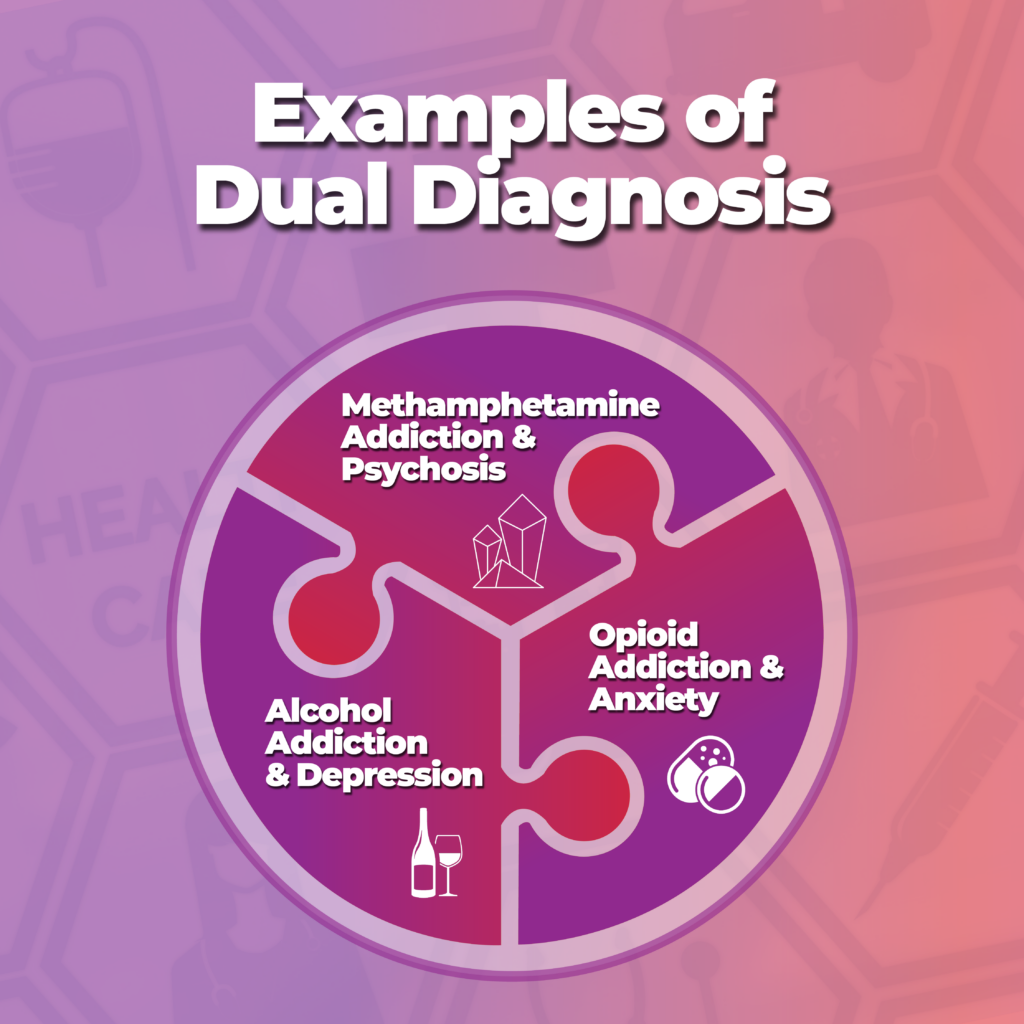
What are Examples of Dual Diagnosis in Addiction Treatment?
Living with a mental health disorder can be a daunting challenge. When combined with substance abuse—a situation often referred to as dual diagnosis—the complexity and hardship can multiply. Dealing with this dual struggle requires a deep understanding of both conditions and their interplay.
In this article, we will explore real-life examples of dual diagnosis in drug and alcohol addiction treatment to illuminate the intricacies of this condition and the pathways to recovery.
Understanding Dual Diagnosis
Before diving into the examples, let’s briefly revisit the concept of dual diagnosis. As we touched upon earlier, dual diagnosis is a term used when an individual is battling both a mental health disorder and a substance use disorder simultaneously. These disorders can be interconnected, with one often exacerbating the other, creating a cycle that can be challenging to break without professional help.
Now, let’s consider some examples that illustrate the nature and impact of dual diagnosis.
Example 1: Alcohol Addiction and Depression
Depression is a common mental health disorder characterized by persistent feelings of:
- Sadness
- Hopelessness
- A lack of interest or pleasure in activities
Alcohol addiction, on the other hand, involves a physical and psychological dependence on alcohol. When these two disorders co-occur, it can lead to a vicious cycle. An individual might use alcohol to cope with the symptoms of depression, such as sadness and hopelessness.
However, alcohol is a depressant, which means it can exacerbate these symptoms in the long run. Moreover, the negative consequences of alcohol abuse, such as relationship problems or legal issues, can further intensify feelings of depression. The co-occurrence of these conditions requires an integrated treatment approach that addresses both alcohol addiction and depression concurrently.
Example 2: Opioid Addiction and Anxiety
Anxiety disorders involve excessive and persistent worry and fear about everyday situations. Opioid addiction, which includes dependence on prescription pain relievers or illicit drugs like heroin, is a serious national crisis that affects public health and social and economic welfare.
An individual with an anxiety disorder might use opioids to alleviate their symptoms, creating a dangerous cycle of self-medication. Conversely, prolonged opioid use can lead to heightened anxiety, especially during withdrawal periods. This dual diagnosis is particularly precarious due to the high risk of overdose associated with opioid misuse.
Example 3: Methamphetamine Addiction and Psychosis
Methamphetamine is a highly addictive stimulant that affects the central nervous system. Chronic methamphetamine use can lead to a host of health problems, including psychosis, a mental disorder characterized by a disconnection from reality.
Methamphetamine-induced psychosis can include symptoms like:
- Hallucinations
- Delusions
- Paranoia
These symptoms can be severe and may persist long after the drug use stops. The co-occurrence of methamphetamine addiction and psychosis presents unique challenges for treatment, given the severity and complexity of the symptoms involved.
The Importance of Integrated Treatment
These examples underscore the complex nature of dual diagnosis and the need for integrated treatment. Integrated treatment involves a coordinated approach to address both the substance use disorder and the mental health disorder simultaneously. This approach is key to breaking the cycle of self-medication and exacerbation seen in dual diagnosis.
What is the most effective treatment for dual diagnosis?
The most effective treatment for dual diagnosis is an integrated treatment approach. This method combines substance abuse treatment and mental health services to address both conditions concurrently, rather than treating them separately. The integrated treatment model is defined by a seamless blending of interventions tailored to the patient’s unique needs, aiming to improve their overall quality of life and reduce the risk of relapse.
An integrated treatment plan for co-occurring disorders could include a combination of:
- Medications
- Psychotherapy (one-on-one)
- Group therapy
- Lifestyle modifications
- Supportive services
For instance, a sample treatment plan might involve:
- The use of medications to manage symptoms of mental illness
- Cognitive Behavioral Therapy (CBT) to address harmful thought patterns
- Group therapy for peer support
- Case management to help with housing, employment, and other social needs.
Integrated Treatment is Not “One-Size-Fits-All”
It’s worth noting that integrated treatment for co-occurring mental health conditions is not a one-size-fits-all approach. Each individual’s treatment plan must be personalized, taking into account their specific disorders, the severity of symptoms, personal circumstances, and treatment preferences.
In terms of specific therapies, co-occurring disorders group therapy can be particularly beneficial. This modality allows individuals to share their experiences, learn from others who are facing similar challenges, and develop healthy coping skills. It’s often used in conjunction with individual therapy and medication management.
There’s also a growing body of resources, like the co-occurring disorders treatment workbook, designed to support individuals in recovery. This type of workbook provides practical tools and exercises to help individuals understand their conditions, develop coping strategies, and stay committed to their recovery journey.
Co-occurring Disorders and Dual Diagnosis in the DSM-5
Examples of co-occurring disorders can be found in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). This comprehensive manual provides a standardized classification and definition of mental health and substance use disorders. Both dual diagnosis and co-occurring disorders are represented within the DSM-5, highlighting their recognition and importance within the psychiatric community.
What is the difference between comorbid and co-occurrence?
The terms ‘comorbid’ and ‘co-occurring’ are often used interchangeably in the medical field. However, there are subtle differences between them that are worth noting. Comorbidity generally refers to the presence of two or more disorders in a person, regardless of the sequence of occurrence or the relationship between the conditions. For example, a person may have both diabetes and hypertension, two conditions that often occur together but are not necessarily caused by one another.
On the other hand, ‘co-occurring disorders’ is a term more specifically used in the field of mental health and addiction treatment. It refers to the simultaneous presence of a mental health disorder and a substance use disorder. The term underscores the mutual interplay between these conditions, with each often influencing the course and prognosis of the other.
Thus, a patient with co-occurring disorders may experience a complex set of symptoms that are different from those of a patient with a single disorder or comorbid conditions.
Co-occurring Disorder Examples
Navigating the world with a mental health disorder is often challenging. When you add substance abuse into the mix—known as co-occurring disorders—the complexity intensifies. To better grasp this dual struggle, we will journey through real-life examples of co-occurring disorders in drug and alcohol addiction treatment. Now, let’s examine some examples that can shed light on the nature and impact of co-occurring disorders.
Example 1: Alcoholism and Bipolar Disorder
Bipolar disorder is a mental health condition characterized by extreme mood swings, including emotional highs (mania or hypomania) and lows (depression). Alcoholism, also known as alcohol use disorder, involves an inability to control drinking due to physical and emotional dependence on alcohol. When these two disorders co-exist, they often exacerbate each other, creating a complex and challenging situation.
A person with bipolar disorder might turn to alcohol to self-medicate, attempting to alleviate the distress associated with their mood swings. However, alcohol abuse can increase the severity and frequency of these mood swings, leading to a destructive cycle. Treatment for this co-occurring disorder must address both conditions simultaneously to effectively break this cycle and support recovery.
Example 2: Opioid Dependence and Post-Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that’s triggered by a terrifying event—either experiencing it or witnessing it. Symptoms may include:
- Flashbacks
- Nightmares
- Severe anxiety
PTSD coils also trigger uncontrollable thoughts about the traumatic event. When PTSD co-occurs with opioid dependence, the path to recovery becomes more complex. Individuals suffering from PTSD might use opioids to numb their emotional pain and distressing memories, leading to a pattern of self-medication.
On the other hand, the withdrawal symptoms from opioids can induce anxiety and stress, triggering PTSD symptoms. It’s clear that the treatment for these co-occurring disorders requires a comprehensive approach that addresses both traumatic experiences and opioid dependence.
Example 3: Cocaine Addiction and Anxiety Disorders
Anxiety disorders are characterized by significant worry and fear that interferes with daily activities. Cocaine is a powerful stimulant drug that has a high potential for addiction. When these two conditions co-occur, it can lead to a relentless cycle of escalating anxiety and increased substance use.
Cocaine users might initially experience temporary relief from anxiety symptoms, leading to repeated use. However, as the effects of the drug wear off, anxiety often rebounds at an even greater intensity. Furthermore, the anxiety associated with obtaining the drug and the fear of withdrawal can also contribute to this cycle. Treatment for these co-occurring disorders needs to simultaneously address cocaine addiction and provide coping strategies for managing anxiety.
Barriers to Dual Diagnosis Treatment
Barriers to the treatment of co-occurring disorders can be numerous and complex, ranging from systemic issues to individual challenges. Systemic barriers might include:
- A lack of integrated treatment services
- Limited access to healthcare
- The stigma associated with mental health and addiction
On an individual level, barriers could include:
- Denial or lack of awareness about the severity of the condition
- Fear of treatment
- Difficulty managing the symptoms of both disorders simultaneously
Despite these barriers, it’s crucial to remember that recovery from dual diagnosis is not only possible but expected with appropriate treatment. The integrated treatment model, which combines mental health and substance use services, has been shown to improve outcomes for individuals with co-occurring disorders. This approach not only addresses the symptoms of both disorders but also focuses on improving the individual’s overall well-being and quality of life.
Understanding the Differences Is Important in Treatment Environments
When dealing with dual diagnosis vs co-occurring disorders, understanding the subtle differences and similarities between the two is vital. Both terms refer to the simultaneous occurrence of mental health and substance use disorders, but they are used in slightly different contexts. Dual diagnosis often refers to this phenomenon in a broad sense, while co-occurring disorders is a term more specifically used within the addiction treatment field, highlighting the intricate interplay between mental health and substance use disorders.
The need for integrated treatment for co-occurring disorders is pressing and evident. The simultaneous management of both mental health and substance use disorders provides the best chance for recovery and long-term well-being. It’s an approach that acknowledges the complexity of these conditions and their profound impact on a person’s life.
Learn More
Whether we are dealing with a dual diagnosis or co-occurring disorders, the focus should always be on providing holistic, integrated care. At Landmark Recovery, we understand the complexities of these conditions and are committed to delivering personalized, comprehensive treatment plans that cater to the unique needs of everyone. With a blend of modern therapeutic techniques, supportive services, and a compassionate, dedicated team, we aim to guide our patients toward a brighter, healthier future. Call 888-448-0302 for 24/7 confidential support.

Choose Recovery Over Addiction
We're here 24/7 to help you get the care you need to live life on your terms, without drugs or alcohol. Talk to our recovery specialists today and learn about our integrated treatment programs.